I crashed my bike on January 5. You can read about the crash here.
After the crash I didn’t realize anything might be wrong. I continued to ride my bike as I usually do. But, on February 20 I noticed that something was not quite right. I went for a 25-mile bike ride that afternoon and noticed a couple of things that didn’t seem right. First, as I was starting the ride, I had a hard time clipping in, so I got off the bike to check if anything was wrong. There was nothing, but when I started to get on the bike I almost fell. If I had been clipped in, I would have fallen. I just felt a little clumsy. Second, on the way back, I felt that it was harder to keep the bike on a straight path–I kept feeling like I was going to run off the road on the right side. With about 1 mile left, I did run off the road but was able to stop without falling.
Four days later on February 24 I went with Ann for a 2-mile walk in the neighborhood. I felt off-balance, and I tended to shuffle my feet. My right leg seemed to drag a little. Ann commented on my awkward walking. I also felt unusually lethargic after the walk. That’s the day I realized that something was definitely wrong with me. That night, I fell while getting up out of a chair. It seemed a little hard to get up. I felt clumsy and my movements seemed slow. Another sign that something was wrong.
The next day on February 25, I felt a little shaky on my feet but was not very concerned. I went to the fitness center and lifted weights without any problems. That afternoon I decided against going for a ride, because my legs felt odd, and I was a little unsteady on my feet. So, I rode the trainer in the garage for about 1 hour. When I started to get off the bike, I swung my leg over the saddle. I fell when my foot hit something next to the bike. I don’t think hitting something with my foot would ordinarily cause me to fall.
The next day, February 26, I decided to ride with the retired riders group. I didn’t feel bad but noticed right away that I tended to veer to the right while riding. We rode across the Big Dam Bridge (BDB), and I had no problem going over the bridge, although I rode slowly. After riding over the bridge and into Burns Park, I realized I could not make the entire ride.
Coreen and Ray were behind me, and Coreen wrote this in an email.
“I was observing you from behind today and you were running to the right. A couple of times, I was afraid you were headed toward the river. I mentioned to Ray that maybe you shouldn’t go up the big hill. That is about when you turned around.”
On the way back to my car, I ran off the trail about 4 time and fell once, though I had pretty much stopped by the time I fell. At the BDB I didn’t find it hard to peddle up the bridge, although I was not going very fast. About ¾ of the way to the top, I fell into the guard rail. I got off and pushed the bike to the top of BDB. I got back on the bike and rode back to my car without a problem. I noticed when I looked straight down while riding, the bike was leaning to the left quite noticeably. When I forced myself to position the bike so it was straight, it didn’t feel right. At the car, I had a hard time getting off my bike. I couldn’t seem to get my leg high enough to clear the seat.
When I got home, I sent my PCP a note on MyChart saying that something was wrong with me and that I needed to see a doctor. He said I should come to the clinic as a work-in with someone or go to the emergency department.
I went to the clinic, hoping to talk to my PCP. After waiting over an hour I was finally able to see the doctor. He examined me but found nothing obviously wrong. I asked him to watch me walk, and he also noticed that the movement of my right my was odd. He arranged for me to have carotid doppler test and an MRI of the brain (scheduled for a month away). He did standard blood tests, which were all normal.
The following 2 days I didn’t do any exercise. By the end of the second day, I decided to go to the ER for a couple of reasons. First, my walk seemed to be worsening, and second I didn’t want to wait a month for the MRI.
It’s not clear to me when I realized that the problems I was having walking and riding my bike were related to the crash I had in January. I don’t think I made the connection at first. But, on the day I rode with the group, Bill, a riding buddy, sent an email to our riding group to say that he was going into the hospital that day to receive treatment for a subdural hematoma. Certainly by then, I figured that my problems were related to the bike wreck. So, when I went to the ER, I had prepared a 2-page summary and timeline of the bike wreck and symptoms I had had.
So, on March 1, I went to the ER at UAMS. We got there about 10:30, and there was nobody in front of us so I went right in. I saw a doctor right away, and he ordered a couple of tests. One was a CT of the head. When the results came back, it was clear to the ER doctor that I had blood on the brain and that I should see someone from neurology.
First Two Holes In My Head
The first person that I saw from neurology (actually from the Neurosurgery Clinic) was a resident who told me I had a subdural hematoma and that I needed to have a procedure to remove the blood. She said there were two possibilities. The least invasive treatment would be to insert tubes in my head to drain the blood. This procedure could be done at the bedside. The other procedure would be done in the operating room, where a hole would be bored in the skull and the blood removed. She said the attending physician would decide the treatment.
The attending physician decided to do the least invasive treatment, which was to put 2 drains in my skull. That procedure would be done at the bedside in the ICU. In the ICU everything was prepared using sterile conditions before the procedure started and cloth was draped over my head and face. During the procedure, I couldn’t see who was in the room or who actually did the procedure. The two doctors I remember being there was a 6th year resident and a first year resident. The person who did most of the talking to me was the first year resident. I’m not sure if she did the procedure but I don’t think the attending physician was there.
After being prepared for the procedure, I had to wait about an hour or more in order to receive an injection of platelets. Since I had been taking a low-dose aspirin, the doctor wanted to minimize the risk of bleeding by giving me platelets. I was also given Fentanyl and Ativan to “take the edge off” and dampen my anxiety during the procedure. The doctor also injected lidocaine in the skin where holes were to be drilled. The procedure didn’t hurt, and I could hardly tell that I was sedated. I heard the drilling, which was loud as promised.

The doctor drilled a hole on either side of my head near the front and screwed in metal drain ports.
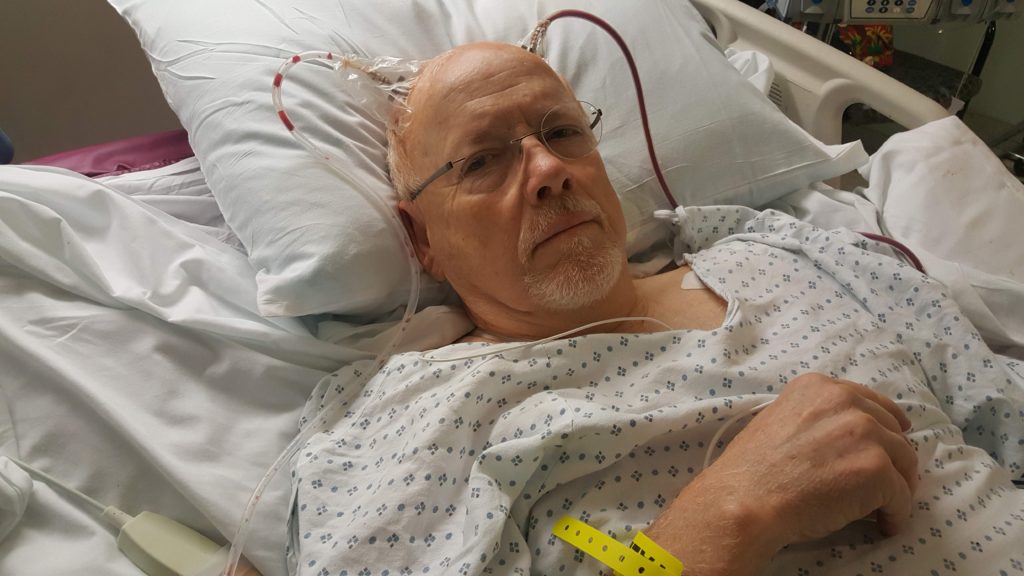
The doctor attached rubber tubes that extended a couple of feet from my head. The tube terminated in an oval-shaped reservoir to collect the blood that drained out.
I wasn’t very worried about the procedure. It’s not rocket science I told myself; it’s drilling. How hard can it be to drill holes in the skull.
WTF! No, it’s not rocket science, it’s brain surgery! If you give me a couple of minutes, I’m sure I can come up with 5 or 6 things that could go wrong. But, by the time the drilling started the Fentynal and Ativan had kicked in, and I was pretty relaxed and mellow. I hoped that the resident had taken a shop class in high school and that she made an A in DRILLING.
I stayed in the ICU for 4 days. I had to lie flat in the bed so the blood could drain out. I was allowed to sit up a little for short periods to eat. As far as I know the only drugs I was given while in the hospital (other than what I usually take at home) was Keppra (an anti-seizure medicine) and Dexamethasone, a steroid. On the fourth day I was started on an antibiotic, because my white blood count was a little low, though in the normal range.
While in the ICU, I got lots of attention from the nurses. They came in my room periodically throughout the day and night to evaluate me by shining a light in my eyes, having me squeeze their finger, move my arms and legs against resistance, and asking me questions. Each day in the ICU I got a CT scan at about 4:00 am. A resident from the neurosurgery group rounded each morning at about 5:30. A doctor from the ICU also came by each day to see how I was doing.
Bedpans and Urinals
It eventually came the time that I needed to use the commode and there was one in my room. So, I asked the nurse if he would help me to the commode. He fetched a bedpan and placed it on the bed and said, no, you must use the bedpan. Seeing the bedpan instantly caused me anxiety, and I started to whine to the nurse. Do you see the size of my ass and the size of that bedpan? There’s no way I will be able to get up on it. Also, not only is it barely wide enough, it appears not be deep enough. I’m about halfway weak with the holes in my head and I’m connected to all these wires. Even if I could get up on it, I don’t believe I can balance myself on it. The nurse said, first, you are not going to get-up-on-it. (Oh, no!) Second, you will have to use the bedpan while lying mostly horizontal in the bed, according to the doctor’s orders. (Really!) When you are ready, let me know and I will help you. Without going into details, it worked out pretty well. It wasn’t his first bedpan rodeo so we made it fine. However, I hope I never have to use a bedpan again!
On the other hand, a urinal for a man is a fine apparatus. Light weight and easy to use without assistance; it can be used without sitting up; and it takes no specialized training to use it. There was always one within arm’s reach on my bed. I even took one home with me when I left the hospital. I put it on the night stand next to my bed. It was reassuring to know, if I woke up at night and needed to pee, I had the option of using the urinal or walking to the bathroom and risk falling. I used it a few times to be sure.
On the last day I was in the ICU, a resident removed the drains from my head. He said he could give me some lidocaine before stitching me up, but he said I probably wouldn’t need it. He was so cavalier about the situation, that I said no, I won’t need any lidocaine. That was a mistake. It wasn’t very painful when he unscrewed the metal drains, but it hurt like hell when he wiped around the drains and when he stitched up the hole.
I was evaluated by an occupational therapist and a physical therapist before I left the ICU. The occupational therapist concluded that I wouldn’t need any assistance after leaving the hospital. The physical therapist thought I had good strength but noted that I was wobbly when I walked.
After the 4th day I left the ICU and spent one night in a regular room for observation. I didn’t get as much attention in the new room as in the ICU, but at least I was able to take a shower.
After five days in the hospital, I went home. I filled prescription for Dexamethasone (a steroid) and Keppra (anti-seizure). The steroid ensured that I wouldn’t sleep very well; I didn’t have a good night’s sleep for a long time.
A couple days after I got home, I called the neurosurgery clinic and asked if I could go for a walk. The answer was yes, but I should go slowly. So, we started to walk several days a week. I was lightheaded and walked pretty slowly and got tired easily. After being home about a week, I started to see improvement. The loss of dexterity in my right hand had improved and I felt stronger when walking and my right leg seemed more or less normal.
About 20 days (March 25) after leaving the hospital I had an appointment for a CT scan. The Sunday before the CT scan on Monday, I had a terrible headache and I noticed that I had neurological symptoms in my left hand—loss of dexterity. After having the CT scan, I went to the ER and explained that I was having problems with loss of dexterity in my hand. I also got an MRI. I was told the CT scan was normal (no change from the last one) and the MRI was also clear (no changes from the last one a few years ago). However, the doctors decided I should spend the night in the hospital for observation. I was moved to an observation ward where several residents from the Neurology Clinic came by and examined me.
I was released from the hospital after one night and got home about 3:00 the next afternoon. About dinner time I received a call from someone from the Neurology Clinic (I didn’t catch her name) who said a final reading of the MRI showed some abnormalities and that I should come to the ER! I told her I had just spent the previous night in the ER and surely this problem could be dealt with the next day. However, after a second thought and a call to my son, the doctor, I took his advice and went to the ER that night.
Big Hole In My Head
The ER was full, and we had to wait a long time. Since I couldn’t remember the name of the doctor that called me, it took some time to track her down. I saw the ER doctor but he said I should see someone from “neuro”. When that doctor from “neuro” came he said it would probably better if someone from Neurosurgery came to assess my case, and he promised to go find someone. Before long a doctor that I recognized from the Neurosurgery Clinic came by. Within several minutes he decided I would need additional surgery. He said there was a little change for the worse that showed up on the CT scan. With several back and forth visits with the attending physician, they decided I should have burr surgery. (Basically a couple of holes bored in the head to flush out the blood.) With that decision we were discharged from the ER. We got home a little before midnight Tuesday night with instructions to wait for a call to schedule the surgery.
The surgery was scheduled for Friday. So, nothing much happened Wednesday and Thursday. My symptoms in my right hand worsened. I seemed more lethargic and slower in my movements. I had unusual headaches. The headaches were in the right frontal lobe and seem to pulsate from time to time, but they were not very severe.
I had to be at the hospital at 5 am on Friday. I bathed using antibacterial soap as instructed. My niece, Sara, the nurse, came to take us. We got there on time, and Sara knew where and how to check in.
It was frustrating from that point on, because we had to wait quite a while before going back to the pre-op area. We spent some time in the pre-op area getting ready for surgery–gown, IV, etc. I was in the OR for several minutes while they prepared things. The last thing I remember was a nurse saying she was going to put a mask over my face.
I don’t remember much about waking up or the early parts of recovery. I don’t remember being in any pain, although I did have a headache off and on for the rest of the day. I took pain medicine (Dilaudid, Tylenol and Morphine, I think) in the morning after surgery. Also, in the evening just before bed I had a dose of Oxycodone.
After several hours in post-op, I was moved to a room. I had a typical night on steroids—no sleep. I rested okay, but I don’t think I slept any at all, until early in the morning.
One of the Chief residents and three other residents rounded about 8:30 the next morning (Saturday). I asked them a lot of questions. Later in the morning, Dr. Rodriguez, the attending surgeon, came by and spent a long time with us. I’m pretty sure she did the surgery. She said they first drilled 2 holes, but because the blood was a very thick clotted mass, they couldn’t extract the blood. So, they cut a larger hole. I said with a jigsaw? She said it was very similar–a lot of our tools are like ones in your garage. She described the saw as having a “foot” on the bottom that went below the skull that acted as a guide to avoid going to deep. After making a larger hole they were able to clean out all the accumulated blood.
While I was still in the recovery room, Dr. Rodrequez showed Ann a picture of the hole in my head she had taken during the surgery. Ann described the hole as a round silver dollar-sized hole. I asked the doctor how the hole was covered. She said they inserted the skull pieces back in place and secured them with tiny titanium screws. It won’t set off alarms at the airport. The surgery was on the left side (left side controls the right side movements). The doctor said the blood that is still left on the right side will probably slowly reabsorb. She also said the “abnormal” area on the MRI was the original hematoma.
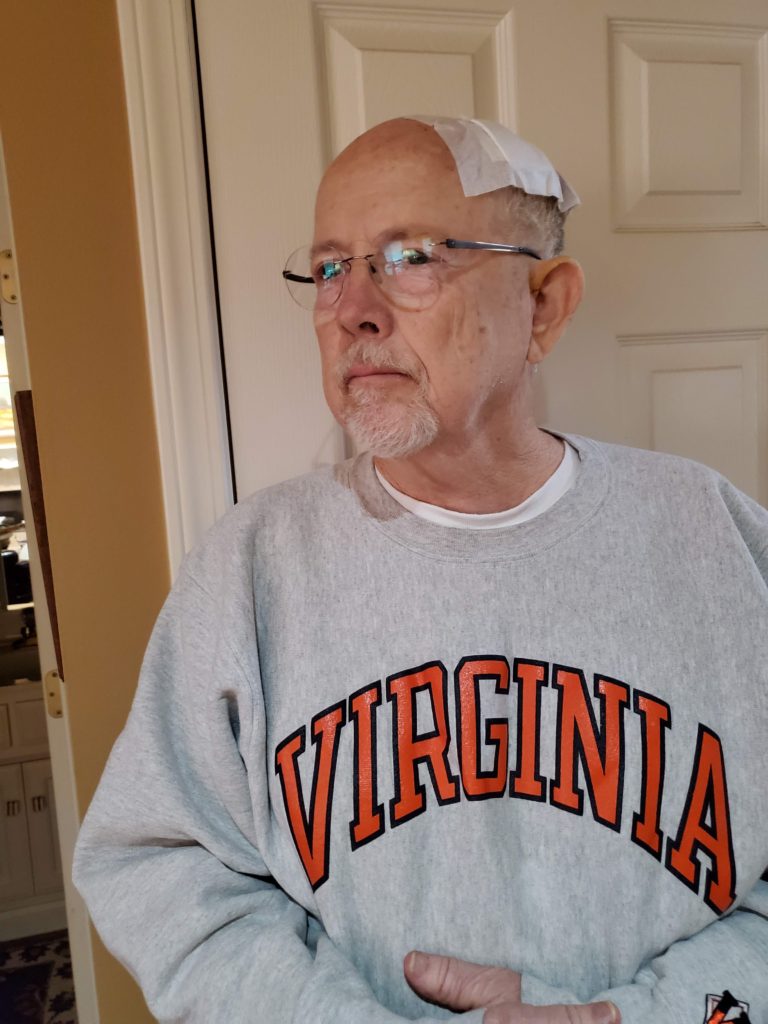
After spending only one night in the hospital, I was discharged with the same instructions as before—no driving, no lifting more than 10 pounds, no bending over from the waist, no pushing, pulling or straining until after I the post-op visit with the neurosurgeon. We got home on Saturday a little before noon. I went home with a dressing over the wound, and I was told to not remove it until the second day, at which time I could gently wash the incision with baby shampoo.

About a week after surgery, I went to see a nurse at the Neurosurgery Clinic, who examined the incision and removed the stitches. I told her that I had been sleeping during the daytime much more than usual. She encouraged me to rest and sleep whenever possible because that would facilitate recovery.
Almost immediately after the surgery, I could tell the dexterity in my hands was much improved. Dr. Rodriguez said it might take a week to for my hands to feel completely normal.
For most of the month after surgery, I still felt weak, I tired easily and I was lightheaded. However, I didn’t have much neurological problems like loss of dexterity in my hands or trouble walking. I had trouble sleeping (I was still taking steroids) and woke up often with a headache. I was prescribed several 5 mg tablets of Oxycodone, and I took several of them or Tylenol at night so I could sleep.
During the first couple of weeks in April I didn’t feel like exercising. But, I gradually started to feel stronger and started walking more often. During the first 2 weeks in May I rode the trainer (stationary bike) in the garage or walked almost every day.
On May 15, I had a CT scan and met with the neurosurgeon. About a week before that I started to feel almost “normal”. The doctor showed me the CT scans before surgery, right after surgery, and the current scan. The before surgery scan showed a lot of blood between the brain and scalp. The scan right after surgery showed a small pocket of blood on the left side, and the last scan showed no blood at all.
Dr. Rodriguez said I could resume normal activities but encouraged me to go slowly. So, the next day I went to the fitness center and rode the stationary bike and lifted weights. The next day I went for a 16-mile bicycle ride! I felt pretty good while riding, though I could tell I was slightly out of shape. I rode 100 miles the week after I saw Dr. Rodriguez.
